NPHIES Taameen
Manages insurance and financial transactions across the patient journey.
Achieve clean eligibility, timely approvals, and denial-free claims powered by a unified NPHIES-compliant HMS that strengthens financial stability for your hospital or clinic.

NPHIES (National Platform for Health and Insurance Exchange Services) is the national framework introduced under Saudi Arabia’s Vision 2030 healthcare transformation to unify how providers and insurers manage eligibility, pre-authorization, encounter documentation, and claims. It establishes a single, standards-based method for exchanging clinical and financial information, ensuring every patient encounter follows a structured and validated workflow.
Manages insurance and financial transactions across the patient journey.
Standardizes clinical and encounter information for accurate documentation.
Built to Support
Optimizes procedure-driven care through
Enables efficient outpatient workflows by
A Unified Journey from Eligibility to Revenue Reconciliation
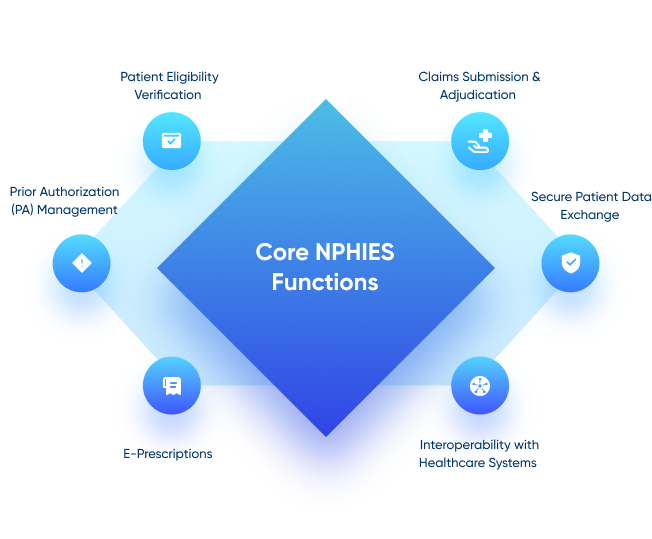
Check insurance coverage instantly with automated NPHIES-compliant verification that support seamless encounters and reduce wait times.

Accelerate care delivery with structured, payer-ready requests that receive faster approvals and minimize insurer follow-ups.

Improve revenue performance with clean, validated claims built for high first-pass acceptance and predictable reimbursement cycles.

Gain full visibility into insurer responses and payment updates in real time—strengthening financial planning and month-end accuracy.

Promote organizational transparency with complete user traceability and easy-to-generate reports aligned with NPHIES documentation standards.

Stay confidently compliant with standardized workflows, unified documentation, and automated reporting that reduce variation across departments.

 Ebook
Ebook
A simple, clear handbook on how NPHIES works inside a modern Hospital & Clinic Management System (HMS)
Download now Ebook
Ebook
Practical guide to selecting an unified, future-ready HMS for smarter hospital operations.
Download now